Difference between revisions of "Glencliff State Sanatorium"
Trickrtreat (talk | contribs) |
Trickrtreat (talk | contribs) |
||
| (2 intermediate revisions by the same user not shown) | |||
| Line 46: | Line 46: | ||
By 1970, other potent new drugs, including rifampin, were also available. That year, Glencliff sent its last active tuberculosis patient to Mary Hitchcock Hospital, ending the sanatorium movement in New Hampshire. The once-flourishing U.S. network of 420 sanatoriums was soon virtually abandoned. Many of the hospitals were eventually converted to other uses, though some were left empty for fear of contagion. In 1970, the Glencliff Sanatorium was converted into the Glencliff Home for the Elderly. Through the efforts of Sandra Knapp, Glenclifff's administrator from 1979 through 2002, and the current administrator, Todd Bickford, many of the unique architectural features of the original facility have been preserved. The main patient building still has its floor-to-ceiling windows that admit ample light and the sturdy columns that used to support the screened porches which were used for the open-air treatments (these spaces have now been framed in, however, to create additional patient rooms). | By 1970, other potent new drugs, including rifampin, were also available. That year, Glencliff sent its last active tuberculosis patient to Mary Hitchcock Hospital, ending the sanatorium movement in New Hampshire. The once-flourishing U.S. network of 420 sanatoriums was soon virtually abandoned. Many of the hospitals were eventually converted to other uses, though some were left empty for fear of contagion. In 1970, the Glencliff Sanatorium was converted into the Glencliff Home for the Elderly. Through the efforts of Sandra Knapp, Glenclifff's administrator from 1979 through 2002, and the current administrator, Todd Bickford, many of the unique architectural features of the original facility have been preserved. The main patient building still has its floor-to-ceiling windows that admit ample light and the sturdy columns that used to support the screened porches which were used for the open-air treatments (these spaces have now been framed in, however, to create additional patient rooms). | ||
| − | + | == Images of Glencliff State Sanatorium == | |
{{image gallery|[[Glencliff State Sanatorium Image Gallery|Glencliff State Sanatorium]]}} | {{image gallery|[[Glencliff State Sanatorium Image Gallery|Glencliff State Sanatorium]]}} | ||
<gallery> | <gallery> | ||
| Line 53: | Line 53: | ||
File:Glencliff-NH-sanatorium.jpg | File:Glencliff-NH-sanatorium.jpg | ||
File:glencliff2.JPG | File:glencliff2.JPG | ||
| + | File:glencliff12.jpg | ||
| + | File:NH01107.JPG | ||
</gallery> | </gallery> | ||
Latest revision as of 15:51, 3 December 2014
 | |
| Established | 1901 |
|---|---|
| Opened | 1909 |
| Current Status | Preserved |
| Building Style | Cottage Plan |
| Location | East Haverhill, NH |
| Alternate Names |
|
History
In New Hampshire, the state legislature authorized construction of a sanatorium in 1901, a year when the state's annual death rate from tuberculosis hit 194 per 100,000 and tuberculosis was the most common cause of death for persons aged 20 to 40. Had tuberculin skin testing been available at the time, virtually every adult would have tested positive—an indication of either latent infection or active disease.
This is in stark contrast to the current situation in New Hampshire. Today, the annual incidence of tuberculosis is 1.6 per 100,000, and fewer than 10% of DMS students have positive tuberculin skin tests (and most of those who do are foreign-born students from countries where tuberculosis is still common). Dartmouth-Hitchcock Medical Center admits only between one and four patients a year with active tuberculosis, and most of them recover after six months of treatment. Dartmouth medical students and residents are more likely to see patients with systemic lupus erythematosus, a chronic inflammatory disease, than with tuberculosis.
The New Hampshire State Sanatorium was located at Glencliff because the site's elevation of 1,650 feet would provide the fresh mountain air that was then thought to be therapeutic for tuberculosis patients. Construction on the facility was completed in the summer of 1909, and the first patient was admitted on September 14 of that year. Dr. John M. Gile, a professor of clinical surgery and later the dean of Dartmouth Medical School, was the first consulting surgeon at the sanatorium, and Dr. Elmer Carleton, also a member of the DMS faculty, was the consulting laryngologist. Most patients came from the major industrial centers in southern New Hampshire, such as Manchester, Concord, and Nashua, but any resident of the state identified as having active tuberculosis would be considered for admission.
Admission required that the patient first be seen by a designated practitioner in Claremont, Dover, Keene, or Manchester or at the sanatorium itself. These physicians were asked to consider whether the applicant presented "a reasonable prospect of improvement or cure" before they referred the patient to the superintendent of Glencliff for admission. Patients with an unfavorable prognosis were usually turned down, though sometimes they would be accepted if it was thought that small children in the patient's home were at risk of infection.
In general, Glencliff did not accept children, although the cutoff for adulthood at the time was 14 years. So-called "pre-tuberculous" and tuberculous children were treated at another New Hampshire facility, the Pembroke Sanatorium, beginning in the early 1920s.
Glencliff's patients came from all social classes and all professions and included doctors, hospital superintendents, factory workers, steamfitters, and junk dealers. For many patients, their stay lasted years, sometimes even decades. A Chinese exchange student at Dartmouth stayed for two years. One patient remained at the sanatorium for 23 years.
In the early 1900s, Glencliff was a self-sufficient community, designed to maintain the isolation that was part of the sanatorium concept. Its medical facilities included a hospital unit, an open ward, an x-ray facility, an operating room, and a microbiology laboratory. The campus encompassed 500 acres and included a farm with pigs and cows and a vast vegetable garden. The institution made its own maple syrup, pasteurized its own milk, and sent summer vegetables to be canned at the New Hampshire State Hospital in Concord. Electricity, water, and sewage disposal were all provided by the nearby town of Glencliff. Coal was brought to the base of the mountain by train until the railroad was discontinued in 1952. The sanatorium even had its own shortwave radio station.
By 1932, more invasive surgical procedures were being used to treat tuberculosis at Glencliff, specifically extrapleural thoracoplasty. This procedure involved the removal of several ribs to bring the chest wall down to the lung and thereby collapse the tuberculous cavity. Patients were instructed to lie on a pillow to push the chest wall against the lung after the ribs had been removed. At least one Glencliff patient subjected to this treatment says that this procedure was very painful and sometimes led to temporary addiction to opiates. Thoracoplasty was observed to reduce the one-year mortality of cavitary tuberculosis from 80% to between 14% and 27%.
Many of the surgical collapse procedures were performed in the single operating room at Glencliff and were done by physicians from Dartmouth, as well as by two surgeons who traveled up periodically from Boston. Dr. Dawson Tyson from Dartmouth performed phrenic nerve resections, thoracoplasties, and extrapleural pneumonolyses during his involvement with the statewide program for the surgical treatment of tuberculosis in the early 1940s. During this time, Glencliff also used Mary Hitchcock Memorial Hospital's pathology and autopsy services, as well as consulting with other specialists from Dartmouth.
Beginning in 1936, intramuscular gold injections were also tried briefly, but were soon discontinued due to the treatment's toxicity and the dif- ficulty of obtaining this German preparation during World War II.
During the pre-antibiotic era at Glencliff, death was a common outcome for patients with chest x-rays that showed the distinct cavities indicative of far advanced disease. The annual reports filed by the institution include statistics on admissions, disease classifications, and deaths—from which it can be calculated that overall mortality rates during the period from 1909 to 1944 ranged from 5% to 22%. An average of 20 patients a year had far advanced pulmonary tuberculosis, and the mortality rate in that group ranged most years between 25% and 45%. And the death rate remained high among patients with far advanced disease even after the introduction of lung-collapse therapy. But the outlook for patients with tuberculosis changed dramatically after the 1944 discovery of streptomycin, the 1946 discovery of paraaminosalicylic acid (PAS), and especially the 1952 introduction of isoniazid.
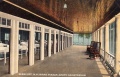
By 1970, other potent new drugs, including rifampin, were also available. That year, Glencliff sent its last active tuberculosis patient to Mary Hitchcock Hospital, ending the sanatorium movement in New Hampshire. The once-flourishing U.S. network of 420 sanatoriums was soon virtually abandoned. Many of the hospitals were eventually converted to other uses, though some were left empty for fear of contagion. In 1970, the Glencliff Sanatorium was converted into the Glencliff Home for the Elderly. Through the efforts of Sandra Knapp, Glenclifff's administrator from 1979 through 2002, and the current administrator, Todd Bickford, many of the unique architectural features of the original facility have been preserved. The main patient building still has its floor-to-ceiling windows that admit ample light and the sturdy columns that used to support the screened porches which were used for the open-air treatments (these spaces have now been framed in, however, to create additional patient rooms).
Images of Glencliff State Sanatorium
Main Image Gallery: Glencliff State Sanatorium