Difference between revisions of "Rockland State Hospital"
m |
|||
| (11 intermediate revisions by 4 users not shown) | |||
| Line 5: | Line 5: | ||
| alt = Rockland State Hospital | | alt = Rockland State Hospital | ||
| caption = | | caption = | ||
| − | | established = | + | | established = 1926 |
| construction_began = 1927 | | construction_began = 1927 | ||
| construction_ended = | | construction_ended = | ||
| − | | opened = | + | | opened = 1931 |
| closed = | | closed = | ||
| demolished = | | demolished = | ||
| Line 14: | Line 14: | ||
| building_style = [[Cottage Planned Institutions|Cottage Plan]] | | building_style = [[Cottage Planned Institutions|Cottage Plan]] | ||
| architect(s) = | | architect(s) = | ||
| − | | location = | + | | location = Orangeburg, NY |
| − | | architecture_style = | + | | architecture_style = Colonial Revival & Mission Style |
| peak_patient_population = | | peak_patient_population = | ||
| − | | alternate_names = | + | | alternate_names =<br> |
| − | Rockland Psychiatric Center | + | *Rockland Psychiatric Center |
}} | }} | ||
| Line 28: | Line 28: | ||
"Much of the staff was drafted during World War II and replaced with nonqualified workers," Sara Fisher, a junior studying psychology at Marymount, said. "Beds were placed in day rooms; infections spread, and there was just one psychologist to care for each 300 patients." | "Much of the staff was drafted during World War II and replaced with nonqualified workers," Sara Fisher, a junior studying psychology at Marymount, said. "Beds were placed in day rooms; infections spread, and there was just one psychologist to care for each 300 patients." | ||
| − | By 1959, the peak year for admittance, Rockland had more than 9,000 residents (including a staff of 2,000). The students, some of whom plan to pursue careers in mental health, studied the history of treating mental illness through archival research and first-hand interviews. At Rockland, insulin shock therapy was begun in 1937, followed by electroshock treatment and lobotomies. The students appeared visibly affected by seeing and handling some of the surgical instruments, all used, their teachers told them, not out of cruelty but as part of what was then considered state-of-the-art treatment. | + | By 1959, the peak year for admittance, Rockland had more than 9,000 residents (including a staff of 2,000). The students, some of whom plan to pursue careers in mental health, studied the history of treating mental illness through archival research and first-hand interviews. At Rockland, insulin shock therapy was begun in 1937, followed by electroshock treatment and lobotomies. The students appeared visibly affected by seeing and handling some of the surgical instruments, all used, their teachers told them, not out of cruelty but as part of what was then considered state-of-the-art treatment. |
| + | |||
| + | Other therapy used was seclusion rooms with a single frosted glass window, a single bed, and a toilet, with a split door with a food service door at the center. Generally three days was the duration given to uncontrollable patients. According to an interviewed patient interned in the early 1940's primarily for being a child that was a discipline problem for her parents, and not having a mental illness, her parents through social services had her interned her at 9 years old for almost a year. Ice sheet baths were given as punishment for unruly, or uncooperative patients, as well as isolation punishments. Also among the girls there was a status social structure that established ones rank through fighting at night. Mostly an open dorm, community bed area was where patients were locked up together at night with staff interacting primarily during daytime hours only. There were 6 cottages for children. Three for girls and three for boys. Also as a non-professional opinion the patient felt that many of her fellow patients were interned due to being physically or mentally abused by family, and we're not diagnosed with mental illness, but became discipline problems, and therefore were made wards of the state. | ||
"In the early years there was very little anesthetic used," Loraine Milosevic, a Marymount junior, said. "They didn't even have teeth clamps to prevent those patients getting lobotomies from biting their tongues." The students learned about treatments for schizophrenia and other mental illnesses, ranging from hydrotherapy ( placing a patient into freezing water in a bathtub to calm the person) to repainting the institution's walls to affect the patient's psyche. (Pink, it turned out, is the most soothing color and today is found in almost all hospitals.) | "In the early years there was very little anesthetic used," Loraine Milosevic, a Marymount junior, said. "They didn't even have teeth clamps to prevent those patients getting lobotomies from biting their tongues." The students learned about treatments for schizophrenia and other mental illnesses, ranging from hydrotherapy ( placing a patient into freezing water in a bathtub to calm the person) to repainting the institution's walls to affect the patient's psyche. (Pink, it turned out, is the most soothing color and today is found in almost all hospitals.) | ||
| Line 36: | Line 38: | ||
Since the 1970's, Rockland Psychiatric Center has served mainly as an outpatient hospital and today houses fewer than 600 patients, primarily the most seriously ill. With the advent of new psychotropic drugs and vocational training, many patients with schizophrenia and manic depression who had been institutionalized are now able to live independently so long as they take medication.<ref>New York Times article: ''[http://query.nytimes.com/gst/fullpage.html?sec=health&res=9D06E4D7153FF930A35752C0A96F958260 Changes In Mental Care],'' January 3, 1999 By DONNA CORNACHIO</ref> | Since the 1970's, Rockland Psychiatric Center has served mainly as an outpatient hospital and today houses fewer than 600 patients, primarily the most seriously ill. With the advent of new psychotropic drugs and vocational training, many patients with schizophrenia and manic depression who had been institutionalized are now able to live independently so long as they take medication.<ref>New York Times article: ''[http://query.nytimes.com/gst/fullpage.html?sec=health&res=9D06E4D7153FF930A35752C0A96F958260 Changes In Mental Care],'' January 3, 1999 By DONNA CORNACHIO</ref> | ||
| − | ==Images== | + | == Images of Rockland State Hospital == |
| + | {{image gallery|[[Rockland State Hospital Image Gallery|Rockland State Hospital]]}} | ||
| + | |||
<gallery> | <gallery> | ||
File:Rockland Psychiatric Center 1987 2.jpg | File:Rockland Psychiatric Center 1987 2.jpg | ||
| Line 42: | Line 46: | ||
File:Rockland State Hospital NY.jpg | File:Rockland State Hospital NY.jpg | ||
File:Rockland SH NY.jpg | File:Rockland SH NY.jpg | ||
| − | |||
| − | |||
| − | |||
| − | |||
</gallery> | </gallery> | ||
| + | |||
| + | ==Cemetery== | ||
| + | The main lot is the burial site for 1,634 mentally ill patients who were institutionalized at Rockland Psychiatric Center in the early 20th century, abandoned by their families or society because of the shame and stigma attached to mental illness at the time. Another cemetery at Rockland Psychiatric Center has 794 graves of people buried from 1965 to the present. The old cemetery, where residents were buried from 1928 to 1965, will be called the Broad Acres cemetery, and the newer one will be named Blaisdell cemetery. Three other cemeteries run by Rockland Psychiatric Center may be refurbished at a later date. | ||
==References== | ==References== | ||
<references/> | <references/> | ||
| + | [[Category:New York]] | ||
[[Category:Active Institution]] | [[Category:Active Institution]] | ||
[[Category:Cottage Plan]] | [[Category:Cottage Plan]] | ||
| − | [[Category: | + | [[Category:Institution With A Cemetery]] |
| + | [[Category:Past Featured Article Of The Week]] | ||
Latest revision as of 19:46, 12 July 2020
| Rockland State Hospital | |
|---|---|
 | |
| Established | 1926 |
| Construction Began | 1927 |
| Opened | 1931 |
| Current Status | Active |
| Building Style | Cottage Plan |
| Location | Orangeburg, NY |
| Architecture Style | Colonial Revival & Mission Style |
| Alternate Names |
|
History[edit]
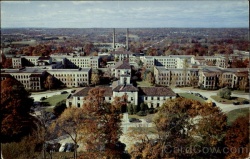
Construction began in 1927 on a 600-acre rural campus, Rockland State Hospital, as it was then known, initially had 5,768 beds. With a working farm, its own power plant and industrial shops staffed by patients who manufactured everything from mattresses to brooms and furniture, Rockland was then considered among the best-planned psychiatric hospitals in the world. In 1931 the hospital opened to 60 male patients, all transfers from Manhattan State Hospital.
"The hospital fostered the idea of the therapeutic suburb," Andrea Bergbower, a sophomore social work major, said. "The thought was that it would be beneficial for these patients to leave the noise and pollution of the city for the isolation of the suburbs to bring them out of their illness." Within 10 years, Rockland's population grew exponentially, along with such attendant problems as overcrowding, disease and staff shortages.
"Much of the staff was drafted during World War II and replaced with nonqualified workers," Sara Fisher, a junior studying psychology at Marymount, said. "Beds were placed in day rooms; infections spread, and there was just one psychologist to care for each 300 patients."
By 1959, the peak year for admittance, Rockland had more than 9,000 residents (including a staff of 2,000). The students, some of whom plan to pursue careers in mental health, studied the history of treating mental illness through archival research and first-hand interviews. At Rockland, insulin shock therapy was begun in 1937, followed by electroshock treatment and lobotomies. The students appeared visibly affected by seeing and handling some of the surgical instruments, all used, their teachers told them, not out of cruelty but as part of what was then considered state-of-the-art treatment.
Other therapy used was seclusion rooms with a single frosted glass window, a single bed, and a toilet, with a split door with a food service door at the center. Generally three days was the duration given to uncontrollable patients. According to an interviewed patient interned in the early 1940's primarily for being a child that was a discipline problem for her parents, and not having a mental illness, her parents through social services had her interned her at 9 years old for almost a year. Ice sheet baths were given as punishment for unruly, or uncooperative patients, as well as isolation punishments. Also among the girls there was a status social structure that established ones rank through fighting at night. Mostly an open dorm, community bed area was where patients were locked up together at night with staff interacting primarily during daytime hours only. There were 6 cottages for children. Three for girls and three for boys. Also as a non-professional opinion the patient felt that many of her fellow patients were interned due to being physically or mentally abused by family, and we're not diagnosed with mental illness, but became discipline problems, and therefore were made wards of the state.
"In the early years there was very little anesthetic used," Loraine Milosevic, a Marymount junior, said. "They didn't even have teeth clamps to prevent those patients getting lobotomies from biting their tongues." The students learned about treatments for schizophrenia and other mental illnesses, ranging from hydrotherapy ( placing a patient into freezing water in a bathtub to calm the person) to repainting the institution's walls to affect the patient's psyche. (Pink, it turned out, is the most soothing color and today is found in almost all hospitals.)
For Dr. Kaiser, who worked at Rockland for 13 years as a psychiatric social worker, going back with her students was also an enlightening experience. "I went in there at the beginning of the process of deinstitutionalization when there were patients who had been there for 30 years," Dr. Kaiser said. "I knew a woman who had been institutionalized since she was 6 years old for epilepsy and didn't even know how to turn on a light. It was very exciting to take students there to learn how far we've come in terms of treating mental illnesses in this country."
Since the 1970's, Rockland Psychiatric Center has served mainly as an outpatient hospital and today houses fewer than 600 patients, primarily the most seriously ill. With the advent of new psychotropic drugs and vocational training, many patients with schizophrenia and manic depression who had been institutionalized are now able to live independently so long as they take medication.[1]
Images of Rockland State Hospital[edit]
Main Image Gallery: Rockland State Hospital
Cemetery[edit]
The main lot is the burial site for 1,634 mentally ill patients who were institutionalized at Rockland Psychiatric Center in the early 20th century, abandoned by their families or society because of the shame and stigma attached to mental illness at the time. Another cemetery at Rockland Psychiatric Center has 794 graves of people buried from 1965 to the present. The old cemetery, where residents were buried from 1928 to 1965, will be called the Broad Acres cemetery, and the newer one will be named Blaisdell cemetery. Three other cemeteries run by Rockland Psychiatric Center may be refurbished at a later date.
References[edit]
- ↑ New York Times article: Changes In Mental Care, January 3, 1999 By DONNA CORNACHIO



